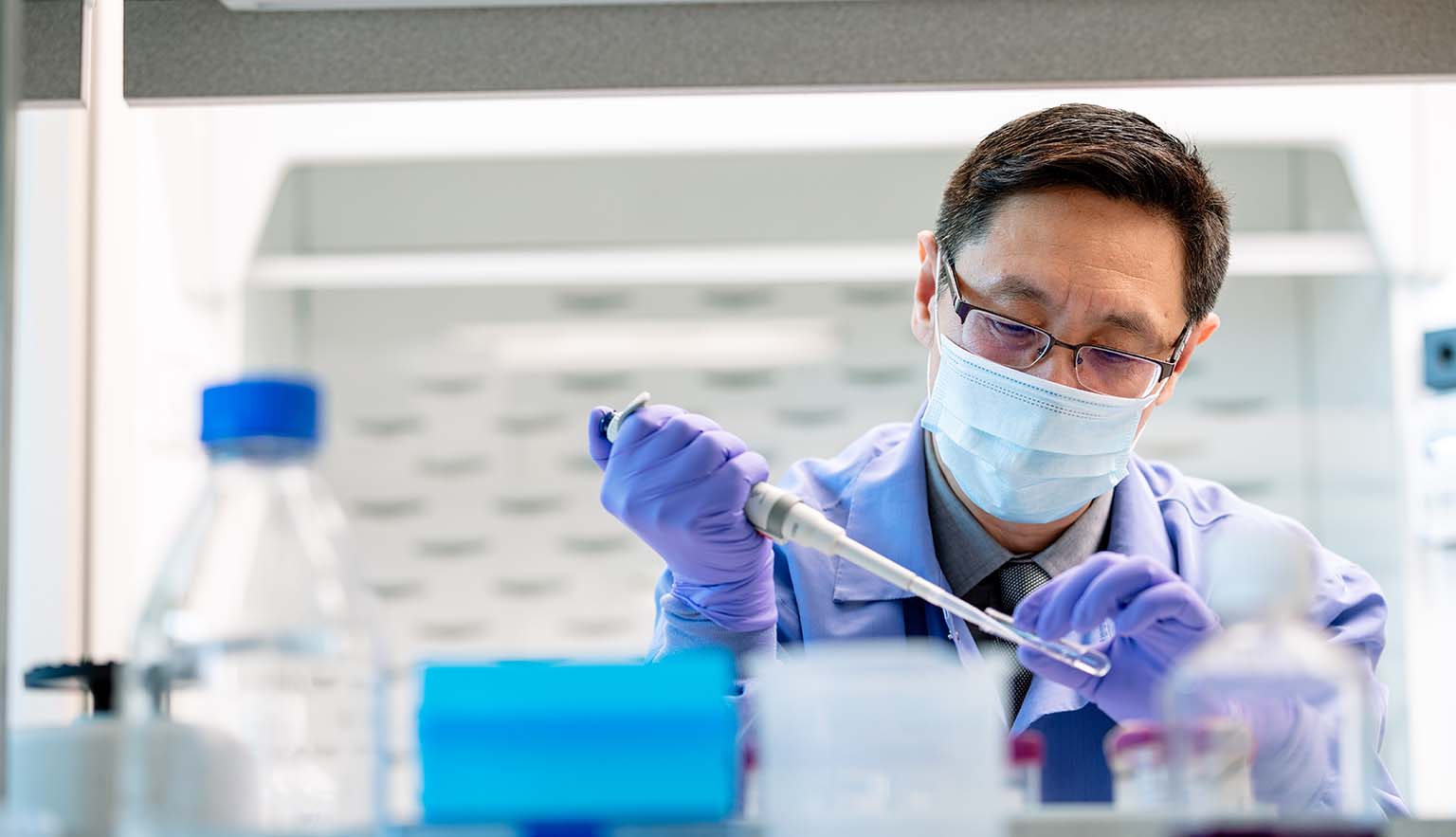
Expanding Immunotherapies Available to Fight Cancers and Other Serious Diseases: One-Minute Interview with Mayo Clinic’s Dr. Hong Qin
February 24, 2021 – By Jared Mueller, Director – Mayo Clinic Innovation Exchange
Emerging immunotherapies — including chimeric antigen receptor (CAR)-T cell therapy for cancer — offer hope to patients around the world confronting certain types of lymphoma, leukemia, and other serious ailments. In recent years Mayo Clinic has constructed several new biotherapy manufacturing and laboratory facilities, all in order to support research and direct manufacturing of these therapies, and to develop new tools to fight other challenging diseases.
Hong Qin, M.D., Ph.D., has joint appointments in cancer biology and hematology/oncology at the Mayo Clinic in Florida campus, where he also serves as director of regenerative immunotherapies. Since joining Mayo Clinic last summer, Dr. Qin has overseen the construction and staffing of specialized immunotherapy manufacturing, laboratory, and warehouse facilities. Dr. Qin spoke with the Exchange about the growth in Mayo Clinic’s immunotherapy research and manufacturing capabilities.
Q: How are plans for biomanufacturing at Mayo Clinic’s Florida campus progressing?
HQ: Currently, we are recruiting the core team who will lead our immunotherapy manufacturing work on the Florida campus. The construction of the Center for Regenerative Medicine’s Advanced Biomanufacturing Facility was completed earlier this winter. The facility has a total CGMP (Current Good Manufacturing Practice, as defined by the U.S. Food and Drug Administration) space of nearly 1,500 square feet. We expect to start the bio-manufacturing of CAR-T products in early 2022.
Q: Can you share a bit more about the details of the biomanufacturing facility?
HQ: Our facility is comprised of three manufacturing suites — with two for CAR-T products, and one for iPSC (induced pluripotent stem cell) products — a quality control lab, office space, and warehouse space. Additionally, a Process Development (PD) lab has been set up to facilitate and optimize the manufacturing process of investigational new drugs. This lab comprises 575 square feet.
The PD lab also houses the same equipment that is used in our GMP manufacturing suites. By procuring the same equipment for both facilities, the generation and efficient transfer of standard operating procedures between the PD lab and the GMP facility will enable us to expedite the manufacturing of clinically acceptable products in the GMP facility.
Q: What would you share with laypeople who may not understand the importance of immunotherapies and specialized biomanufacturing facilities, in terms of how these developments might improve their (or their loved ones’) care someday?
HQ: Not all that long ago, when I was starting out as a physician, certain types of cancer were perceived to be incurable. Today, we’re seeing immunotherapies deliver long-term survival to many patients with blood cancers who previously had little hope.
By developing new facilities that accelerate the “bench-to-bedside” translation of emerging therapies — enabling them to start clinical trials and reach patients months or even years earlier than they would have otherwise — we have the potential to extend and improve the lives of many patients who otherwise may not have received these therapies in time.
As someone with seven patents around CAR-T and antibody technology, and who is involved in a number of innovations currently undergoing clinical trials, I’m very motivated by work that helps groundbreaking science serve patients who are anxiously awaiting life-saving therapies.
Q: What breakthrough innovations in healthcare delivery or technology excite you most?
HQ: When CAR-T therapy is highly successful against hematological malignancies; however, diseases remain incurable due to emerging relapse and refractory tumors that become resistant to treatment. Cutting-edge technologies are highly demanded to improve CAR-T design. Among the newly developed, innovative technologies, “Gene Editing” and “Single Cell RNA Seq” are the most impressive ones related to CAR-T research.
The former technology paves the way to development of allogenic CAR-T therapy, which in turns makes CAR-T therapy accessible to many more patients. The “Single Cell RNA Seq” technology enables us to learn what happens to the CAR-T cells in a patient’s body. The knowledge obtained will guide us to design the next generation: armored CAR-T therapy which aims at curing cancer patients.
Call for Oncology and Immunotherapy-Related Innovations
Are you developing innovative cancer treatments? Contact the Mayo Clinic Innovation Exchange to learn how membership can help bring your company or your idea closer to patients.